|
|

ADAPTIVE IMMUNE RESPONSES
Memory Cells
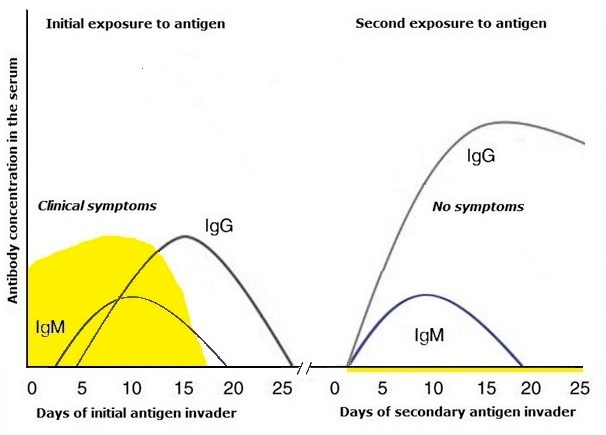
Some lymphocytes are destined to live on as memory T cells, memory B cells, and long-lived plasma cells. These long-lived and even lifelong lymphocytes will protect the body against repeated attacks by the same pathogen. Due to these subsets of memory cells, immune responses to subsequent infectious pathogens are faster and highter than the first response. The functioning of memory cells explains why once a human has had an infection, he or she does not get this infection when exposed to it the next time around. Prior vaccination also results in the formation of memory cells. As a rule, lifespan of memory T and B cells is lifelong.
About 40% of B cells in adults are memory B cells, and several subsets have been identified. Besides IgG+/IgA+ memory B cells, half of the peripheral blood memory B cells express IgM often without IgD. Reactivated IgG B cells differentiate directly into plasma cells. A common phenotypic marker of memory B cells is IgD- IgM+IgG+IgA+CD27+.
For 1.5 years, long-lived plasma cells provide an additional mechanism of maintaining antobodies production with no repeated antigen stimulations.
Memory CD4+ and CD8+ T cells, along with effector T cells are end-cells after T-cell-mediated adaptive immune responses complete. Central memory T cells (TCM) present in the peripheral lymphoid organs and bloodstream and effector memory T cells (TEM) located in the barrier organs are well-chatacterized memory T cells.
TCM cells express CD45RO+, CD27+, CD28+, CD62L+, CCR7+, IL-2+ while TEM cells display CD45RO+, CD27+,CD28+, CD62L-, CCR7-, IFN-γ+, TNF-β+. See more information at flow cytometry gating.
In addition, the other memory T cells, tissue-resident memory T cells (TRM) and stem cell memory T cells (TSCM) are identified.
In elderly persons, there are more memory T cells and fewer naïve T cells that decrease in potency to initiate immune responses to new antigens. The SARS-Cov-2 infection in older people is the same case.©V.V.Klimov