|
|

ATOPIC ALLERGIC DISEASES
Food Allergies
Food allergies are linked to IgE-dependent hypersensitivity to food proteins, particularly those derived from the "Great Eight." In addition, there are other food allergies phenotypes such as IgE-independent and pseudo-allergic (i.e., immune system-independent), of which mechanisms contribute to the food allergy challenges. Patients of this polymorphic condition may develop isolated itching, urticaria, angioedema, bronchospasm, and life-threatening anaphylaxis. Having the immature maintenance mechanisms of natural tolerance to food proteins, children at an early age suffer from food allergies more often than grown-up persons. However, it is estimated that 5 % of children under four years of age and 3 to 4 % of adults in industrialized countries have food allergies.
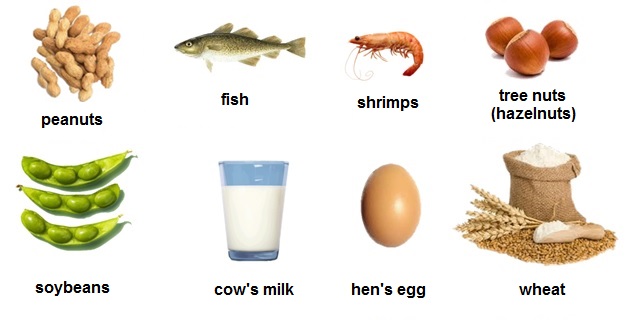
There are three classes of food allergens. Class 1 food allergens includes oral allergens such as cow's milk, peanut, hen's egg, etc. that cause sensitization via the gastrointestinal tract and display severe clinical symptoms. Class 2 food allergens consists of allergens like apple, celery, carrot, melon, and kiwi, which are cross-reactive with aeroallergens, evoke sensitization via the respiratory tract and exert not severe cross-reactions named "oral allergy syndrome." Class 3 food allergens contains small food proteins < 10 kDa, additives, colorants like tartrazine, and contaminants, which frequently cause occupational allergies.
Immunopathogenesis. A food allergen enters the body via the (1) gastrointestinal tract, (2) respiratory tract, (3) skin, or even (4) genitourinary tract. The epithelium generates alarmins, IL-25, IL-33, and thymic stromal lymphopoietin (TSLP), upregulating group 2 innate lymphoid cells (ILC2), allergen-presenting cells, and Th2 cells. Activated ILC2 secrete IL-5, IL-9, and IL-13 affecting eosinophils and mast cells. Food allergen is engulfed by submucosal dendritic cells (DCs), processed, and presented to Th2 cells that trigger Th2-controlled B-cell response with IgE end-production promotion and memory B and memory T cells formation. If an allergen entered via the gut the process proceeds in Peyer's patches. Th2 cells produce type 2 cytokines such as IL-4, IL-5, IL-9, IL-13, and IL-33 and drive allergic inflammation. IL-33 is essential for the maturation of mast cells. Follicular helper T (Tfh) cells secrete IL-21, IL-4, and IL-13, important for upregulating IgE class switch recombination in B cells, maturing plasma cells, and growing allergen-specific IgE affinity. Since the enteric nervous (ENS) system fills in pro-tolerogenic neurotransmitters, food allergen cannot easily overcome the system of allergen tolerance maintenance. However, if it happens, allergic inflammation develops, and food allergies manifest.
Treatment management includes educating the patient about the strict allergen avoidance,prescribing biologics, and the method of oral allergen-specific immunotherapy (AIT). In severe cases, an epinephrine auto-injector should prescribe. Currently, research on oral AIT is at the cutting-edge, and FDA (USA) has approved the first licensed oral AIT product for peanut allergy - Palforzia® (2020).
Prevention. The approaches to the early introduction of allergenic foods in infants are still in progress.
©V.V.Klimov